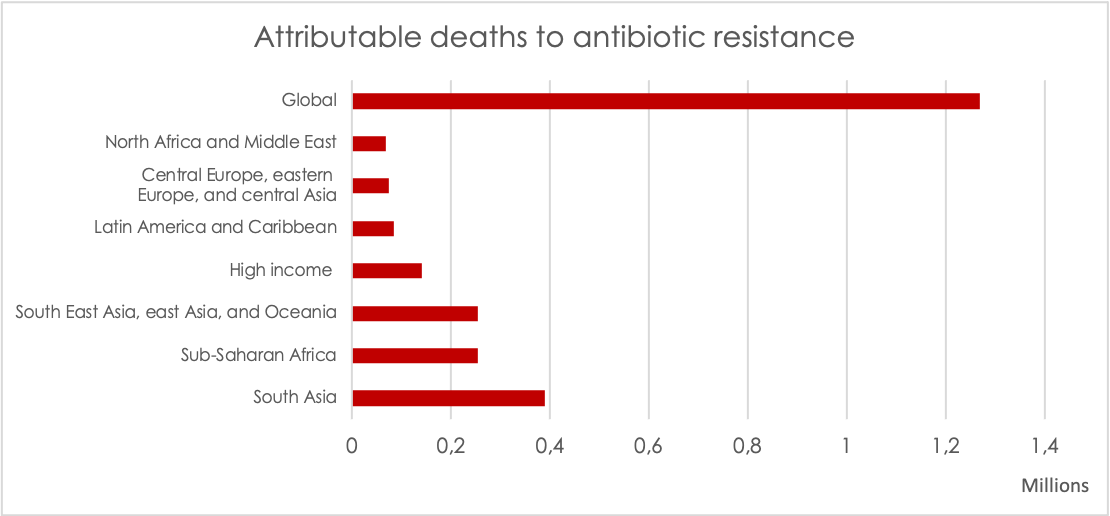
Causing 1.27 million deaths per year, antibiotic resistance is one of the greatest and most urgent cross-border public health threats of our time. However, the global community was late to the table to pick up on the systems failure of antibiotic resistance. Initiatives and collaborations have been initiated since 2015, but stronger globally coordinated governance is needed to drive systemwide response. There is still a long way to go. In this article, you get an overview of the global governance considerations for antibiotic resistance.

Antibiotic resistance is one of the greatest and most urgent cross-border public health threats. However, the global community was late to the table to pick up on the challenges of antibiotic resistance. It was not until 2015, the World Health Assembly adopted the Global Action Plan on Antimicrobial Resistance (GAP AMR) and urged countries to develop National Action Plans. In 2016, antimicrobial resistance was featured at the high-level meeting of the UN General Assembly with the resulting political declaration. Alongside various initiatives following the political declaration, the ad-hoc Interagency Coordination Group (IACG) delivered recommendations to the UN Secretary General in 2019 on approaches needed to ensure sustained collective global action. However, hard-built political momentum has been waning and substantial shortcomings remain in political commitments, financing and international collaboration on response to antibiotic resistance.
Review of GAP AMR identifies critical gaps
In September 2021, six years after the adoption of the GAP AMR, WHO completed and released the Comprehensive Review of the Global Action Plan on Antimicrobial Resistance (GAP AMR). It identifies critical need for greater coordination with international and national partners, slow progress on establishing an AMR global governance structure, lack of coordination across these structures, and lack of progress in mobilizing financial resources for implementation. Apparently, there is much to be done to achieve the governance goals set out in the GAP AMR and subsequent efforts, such as the IACG recommendations.
Global health a top political priority – opportunity to address need for resilient health systems

As global health has become a top political priority during the COVID-19 pandemic, the world now has an unprecedented opportunity to address the unveiled need for resilient health systems that are highly dependent on effective antibiotics. The recent release of the global burden of antibiotic resistance also presents an impetus for speeding up actions on multiple levels with much stronger global commitments. Effective and sustainable global governance is imperative for systemwide response to antibiotic resistance. A long-term goal for addressing antibiotic resistance should be to protect antibiotics as a global public good while ensuring appropriate and sustainable access to effective antibiotics for everyone, everywhere.
Principles for an effective global governance mechanism
Effective global governance on antibiotic resistance should take a front-facing role to:
- provide leadership,
- advocate for political will,
- promote social and resource mobilization, and
- address the challenging barriers for innovation of needed technologies such as new treatments, diagnostics and vaccines.
The establishment of a governance structure for antibiotic resistance should ensure international legitimacy to deliver rules and guidelines that can be judged equitable and inclusive, while common rules, priorities and binding commitments need to be contextualized to the resource settings.
An approach to such a governance mechanism needs to ensure principles of transparency and fairness. A genuinely transparent process should aim beyond just ‘check-the-box’ type of public consultations and provide meaningful opportunities for exchange and responsiveness to concerns raised. Fair representation requires adequate resources for civil society and for low- and middle-income countries to participate and engage in the process. The principles also extend to the policy making process. Both the inputs and the outputs of the intergovernmental process of shaping global governance decisions require transparency as well as efforts to safeguard against financial conflict of interest. Building consensus should be shaped by evidence and by monitoring for accountability, and not by industry’s special interests.
Last but not the least, the mobilization and prioritization of funding must be tied to the public needs; therefore, the governance mechanism should also have a role in both ensuring that the global financing mechanisms function properly, and that priorities are set across sectors based on context, including prioritization based on proportionate responsibility for the use of antimicrobials, particularly in pharmaceutical manufacturing, healthcare delivery or food system delivery.
Key considerations for global governance functions
Resource mobilization for national actions
In order to achieve a real change, countries must make individual and collective commitments for action through a range of cross-sectoral actions and investments. One essential function of a global governance mechanism is to promote, facilitate, and support national level action. The resources, capacity, and knowledge needed to implement and sustain action differ across countries so there is a need for global support in providing funding, normative guidance, and technical assistance. Meanwhile, countries must be held accountable for the commitments made and progress should be monitored and reviewed at both national and global level.
Lack of financing has been acknowledged as a major obstacle for national actions and this situation will likely worsen due to the negative impact of the COVID-19 pandemic on health systems and the global economy. New global burden data on antibiotic resistance clearly show the current magnitude and geographical dispersion of the antibiotic resistance hazard. While many low- and middle-income countries have developed National Action Plans, the Tripartite AMR country self-assessment survey found that only one out of five National Action Plans had been adequately financed and implemented. Tangible funding for national actions needs rapid expansion.
Addressing antibiotic resistance has not been visible in the global financing landscape nor in main funding streams. While the establishment of the Multi-Partner Trust Fund in 2020 has been a positive first step, commitments from only 4 countries (The Netherlands, Sweden, UK and Germany), and the roughly 19 million USD pledged up to now, are far from matching the actual needs. The IACG recommendations urged existing financing mechanisms, such as the Global Fund to Fight AIDS, Tuberculosis and Malaria (the Global Fund), to give the antibiotic resistance issue greater priority in their resource allocations, including assessing the need to expand their scope and mandate.
Recently, the Lancet also published an editorial calling for the Global Fund to include antimicrobial resistance (AMR) in their strategic areas:
“The existing burden of AMR and its future threat should be an urgent stimulus to revise and widen The Global Fund’s mission. It is now time for the Fund to embrace AMR as one of its core responsibilities”.
Policy coherence across sectors and agencies
Antibiotic resistance as a multi-sectoral systems issue cuts across multiple international and national agencies. To build policy coherence and overall political will, it is crucial to reframe the narrative for antibiotic resistance as a systems issue and a development challenge. For effective and sustainable response, a global governance mechanism will need to enable a broader remit of action and be able to influence a wider set of relevant policy agendas on sustainable development.
Deliberations from IACG discussion paper on Governance (July 2018):
- Have a clear One Health mandate to elevate global action on AMR across human and animal health, agriculture, food, and environment, supporting the translation of this action to the national level. This mandate requires backing from senior leadership across all sectors, calling for AMR to be considered as ‘core business’ and holding Member States to account.
- A viable governance mechanism should play a key role in convening different groups and must bring all AMR stakeholders to the table, engaging with Member States, ensuring representation and involvement of low-and middle-income countries by including these voices at every level, recognizing resource and context needs.
- Integrate with the wider global development agenda to better align on and mobilize actions that create common good. It is clear that many objectives for addressing AMR would also provide wider public good, particularly across the sustainable development agenda.
A truly One Health approach requires engaging other key international agencies beyond the Quadripartite (WHO, FAO, WOAH and UNEP), and other UN agencies as core partners through the UN sustainable development cooperation framework and a whole-UN approach to antibiotic resistance. It requires aligning the normative guidance and the priorities of different UN and intergovernmental agencies as well as coordinated efforts through systematic and meaningful engagement of civil society organizations as key stakeholders in the One Health response to antibiotic resistance at global, regional, national and local levels.
Filling the evidence gap
Information transparency and openness are key to building public knowledge of the true scale of antibiotic resistance as well as monitoring for accountability to the public’s interest. Independent and sound evidence is a well-acknowledged dimension of an effective and credible policy development process, and it is an important aspect of global and national governance on AMR. High quality monitoring relies on the availability, collection, and analysis of reliable national data. This begins with collecting and making publicly available the data on antibiotic use, drug resistance patterns, price, and measures of access and stewardship. Independent assessment of available evidence and the capacity to invest in gap-filling research are also important to the process of antibiotic resistance governance.
Global burden of antibiotic resistance
In January 2022, the most comprehensive data to date on the global burden of antibiotic resistance was published in the Lancet. This is the first time that long-awaited global burden data are available presenting a full picture of the spread of antibiotic resistance and its overall health impact. An estimated 1.27 million deaths were a direct result of antibiotic resistant bacterial infections in 2019. Compelling evidence shows that antibiotic resistance is not a future threat – it is here now as a leading cause of global mortality with a magnitude exceeding that from major infectious diseases such as HIV or malaria. The study also indicates that the burden of antibiotic resistance falls disproportionately on low- and middle-income countries. One take-away from this is that we need to prioritize better how to tackle antibiotic resistance challenges in different contexts, e.g. places where there has been high human antibiotic use and high resistance versus low antibiotic use and high resistance. While the newly published data is great progress filling in the evidence vacuum in the current magnitude of antibiotic resistance threats, there is still a lack of comprehensive data on antibiotic use, drug resistance patterns, price, etc. that can guide meaningful national strategies.
Reforming the innovation system with a needs-driven end-to-end approach
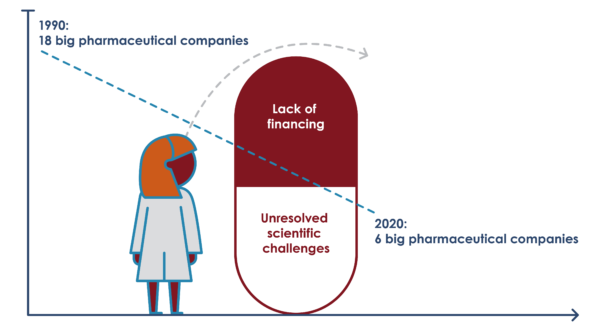
Over three decades of standstill in antibiotic innovation is convincing evidence that the world cannot continue to leave it to ‘the market’ to develop antibiotics. Major scientific challenges continue in early stages of drug discovery, and financing for preclinical and clinical development are neither sufficient nor targeted enough. According to the WHO 2020 review of the clinical and preclinical antibacterial pipelines, 81% of preclinical pipeline continues to be dominated by micro-size (<10 employeed) and small-size (<50 employees) institutions. While the antibiotic pipeline remains unresponsive to global needs, global and national discussions need to move away from focusing on “market fixing” which often limits discussions to only focusing on how to re-enlist the big multinational pharmaceutical companies within the constraints of their traditional business model. Governments have to start seriously considering the alternatives, and start exercising far stronger public leadership in testing new ways to overcome the actual challenges.
Public leadership with novel approaches required
Novel approaches are required at all stages from early research and development to patient access. In the past 5 years, normative guidance, notably the WHO Priority Pathogens List has been developed with the aim to ensure that antibiotic research and development is needs-driven. Although public and philanthropic investments supporting the development of antibacterial compounds have increased, coordinated public sector engagement with vision and intent is required to solve multiple shortcomings throughout the whole system. Clear public leadership is to define a needs-driven, end-to-end vision for development of and sustainable access to effective new antibiotics. New alternative and transformative models of financing, collaboration, IP management, production, procurement and distribution need to be explored.
A delinked pharmaceutical Research and Development model
Paying companies for their R&D investments upfront, means these investments do not need to be recouped through sales profits. Low-cost production and public health driven distribution models can therefore be established from the day the drug receives market authorization. Infograph by Zellout. Click infograph for enlargement.
A crucial part of such models is delinkage, which has been acknowledged for its potential to ensure affordable access without excess use of antibiotics and highlighted in the landmark UN Political Declaration on Antimicrobial Resistance in 2016:
”We acknowledge the importance of delinking the cost of investment in research and development on antimicrobial resistance from the price and volume of sales so as to facilitate equitable and affordable access to new medicines, diagnostic tools, vaccines and other results to be gained through research and development.”
This approach has yet to be implemented in a globally coordinated manner. Increased focus must be given to the formidable challenge of introducing new antibiotics into health systems without propagating the historical mistakes of overuse and misuse of antibiotics while ensuring equitable access.
Reforming system to address global health inequalities
The COVID-19 pandemic has exposed systemic and deeply unacceptable global health inequalities. In this regard, the overall broken model for antibiotic R&D offers an opportunity to build back better for the global community by creating a comprehensive end-to-end model which by design is intended to serve the health needs of rich and poor. This also means that low- and middle-income countries must have a seat at the table when rules are set and priorities are made to ensure that no one is left behind. There is an urgent need for governments to jointly define and take an end-to-end approach towards reforming the system to ensure affordable sustainable access to antibiotics for everyone, everywhere, which implies that new antibiotics should be available, affordable and managed to preserve their effectiveness for as long as possible in all countries.

Affordable sustainable access to antibiotics for everyone, everywhere
While the world is caught up in responding to the COVID-19 pandemic, it has gone largely unnoticed that more than thirty years has passed since the last class of antibiotics was discovered. Meanwhile global consumption of antibiotics continues to increase. In response, bacteria have developed resistance and are spreading as a silent but steady pandemic threatening to devastate healthcare and modern medicine as we know it.
Reflections on the current status of global governance structure on AMR

The ad hoc Inter-Agency Coordination Group on Antimicrobial Resistance (IACG) findings in 2019 suggested that a global, multi-stakeholder agreement is urgently needed to provide a sufficient mandate to act in accordance with the needs identified, providing the authority to coordinate resources, engage stakeholders, and secure binding commitment for action. It recommended constituting a One Health Global Leadership Group (GLG) on AMR; an Independent Panel on Evidence for Action against AMR; and a multi-stakeholder partnership platform to address the breadth of sectoral interests in AMR governance. The IACG report also calls for “provision of political, financial and technical support for civil society organizations to enhance their engagement”.
However, 3 years after the IACG recommendation and over five years since WHO adopted the Global Action Plan on AMR (GAP AMR), the AMR governance structure has not come together in a way that engages the breadth of international agencies that must be engaged, mobilizes financing required for carrying out its work, nor ensures the necessary accountability to deliver on the GAP-AMR, as highlighted in the recently published briefing note “The Global Action Plan on Antimicrobial Resistance (AMR) at a Crossroads – Insights from the WHO’s Comprehensive Review” by the Antibiotic Resistance Coalition.
The AMR Global Governance Structure
The AMR Global Governance Structure
Following the IACG recommendations, a fledgling governance structure has been slowly emerging at the global level. The current global AMR governance structure comprises mainly the Quadripartite agencies – WHO, FAO, WOAH (founded as OIE), and with recent involvement of UN Environment Programme (UNEP)–. However, this structure neglects other international and UN agencies, such as the UN Development Programme (UNDP), the UN Children’s Fund (UNICEF), and the World Bank which have a stake in the multi-sectoral issue of AMR containment and can provide technical and financial resources, a better align on and mobilize actions through wider global development agenda.
While the proposed global governance structure continues to unfold, ReAct had recommended that all three parts of the governance mechanism be established together, to make sure lines of accountability were clear and that all parts can be synergized into a larger whole. The creation of the GLG was a welcome step, but it remains captive to the Tripartite agencies. The GAP-AMR Comprehensive Review also pointed out that :
“it is difficult to assess details of how (these groups) interact among themselves and with other mechanisms, and the anticipated cost, it does seem that there could be a risk of the global governance and coordination mechanisms being too cumbersome, bureaucratic and costly”.
AMR global governance must improve accountability
To be effective, the GLG must both be seen as holding the Tripartite agencies accountable and also making a compelling case, based on benchmarking that progress, for greater financing to advance that mission. It is worth reiterating that AMR global governance must engage all stakeholders, but in so doing, resist the undue influence of those with financial conflict of interest. Strengthening representation and voice of civil society, of low- and middle-income countries, and of future champions for AMR in global governance structures will improve accountability and responsiveness to public health priorities.
Independent Evidence Panel requires follow-through on principles and roles
The establishment of an Independent Panel on Evidence for Action on Antimicrobial Resistance is a key recommendation from the IACG that requires follow-through. Such an independent evidence panel is needed to provide robust and authoritative assessments of the science, data and evidence related to AMR across all sectors, assess its impacts and future risks and recommend options for adaptation and mitigation to governments and all stakeholders. It is instrumental that the approach by which it is implemented and how it functions, ensures independence, as this is critical to its success, credibility and strategic value to global governance. However, the proposed terms of reference for the Independent Panel neither make it independent of the Tripartite agencies, nor is it yet operational. Role of the independent panel in governance and principles behind were further elaborated in the feedback submitted by the Antibiotic Resistance Coalition.
Structure and governance for Multi-Stakeholder Partnership Platform concerning
More recently, the proposed structure and governance for a Multi-Stakeholder Partnership Platform on AMR has stirred concern that the take-aways from the Comprehensive Review have not been heard. As pointed out in the public discussion feedback, collective engagement limited by consensus among those with financial interests (e.g. the private sector) that run contrary to public health concerns could both distract and waste limited resources. The ambition of the Platform seems more focused on recruiting 200 stakeholders than building a coalition of the willing, providing them the “political, financial and technical support” to take action, and lifting up the voices from civil society and low- and middle-income countries which may not otherwise be heard. Finally, the Platform calls for accountability to the Directors-General and the governing bodies of the Tripartite agencies when, in fact, the Platform should be empowered to hold the Tripartite and other implementing agencies accountable for meeting milestones and making progress on the global AMR agenda.
Act Now, while forward-looking to a resilient future: inclusion of antibiotic resistance to Pandemic Preparedness and Prevention

It is time to act now. A leading cause of death worldwide with a burden higher than that of HIV/AIDS or malaria, antibiotic resistance is an ongoing pandemic with severe long-term socioeconomic impact. Aside from the striking number of 1.27 million deaths directly attributable to antibiotic resistance, the World Bank report underlined the economic and development consequences including millions of people being pushed into extreme poverty and trillions of economic losses if antimicrobial resistance remains unchecked. The World Bank analysis also indicates that urgent action on antibiotic resistance constitutes one of the highest-yield investments and more than 80% of the benefits from antibiotic resistance investment would be returned to high-income and upper-middle income countries, a fact that should further motivate governments to make robust and comprehensive investment into antibiotic resistance now.
COVID-19 lessons: swift R&D possible, and rules-based global governance critical
While unprecedented mobilization during the COVID-19 pandemic has led to swift development in advancing diagnostics and vaccines, it has also exposed the limitations of global collaboration and compliance within the existing global health frameworks, pointing to a clear need for more rules-based global governance to be able to effectively prevent, prepare and respond to health emergencies in a more just and equitable way. While COVID-19 has disrupted routine healthcare delivery and displaced resources that would have benefited antibiotic resistance containment efforts, it has also provided a window of opportunity to root antibiotic resistance in the unprecedented scale-up of global efforts to address pandemic preparedness, prevention and response.
Pandemic preparedness needs a broader view
Building on the current political momentum, it is important that the efforts now do not become too narrowly focused on addressing “another coronavirus epidemic,” but takes a wider view on pandemic preparedness. Inclusion of antibiotic resistance to a new international legal instrument was made an advocacy priority by the Global Leaders Group on AMR. The upcoming intergovernmental negotiating body discussions around international legal instrument – pandemic preparedness and prevention should consider antibiotic resistance in the context of pandemic preparedness efforts – both as it relates to the revision of the International Health Regulations, as well as in the context of the new legal instrument. In a wider context, it is expected that the negotiations should also incorporate effective measures on antimicrobial stewardship and sustainable access. To achieve a sustainable path forward to address current and future pandemics cornerstones such as transparency, needs-driven research and development, and above all – equity should be at the center of efforts to establish a new global agreement.
Several elements of an effective global system for pandemic prevention, preparedness and response are in common with what is needed to addressing antibiotic resistance, including:
- Developing medical countermeasures and new antibiotics both require a health-needs driven research and development model.
- Pandemic prevention and preparedness and addressing antibiotic resistance both require taking a One Health approach.
- Improved global surveillance is required for both viral and bacterial infections.
- Increased transparency of global pharmaceutical supply chains and strengthening regional production capacity.
- Ensuring equitable, affordable and timely access to health commodities.

ReAct Europe briefing note on pandemic treaty and antibiotic resistance
On 29 November – 1 December, the 74th World Health Assembly (WHA74) gathered for a special session to consider developing a new WHO convention, agreement, or other international instrument on pandemic preparedness and response. Ahead of the session, ReAct Europe developed a briefing note outlining key considerations that are imperative for making negotiations of a new legal instrument productive for all actors involved.
Download ReAct Europe briefing note: The Pandemic Treaty and antibiotic resistance (PDF)
The world is vulnerable to a pandemic of resistant infections

Here you see Kachia, Kaduna State – September 6, 2021: Young African Recovering on a Sick Bed in a rural clinic After a Successful Surgery. Photo: Shutterstock.
The world must be aware that decades of funding neglect, combined with continuously increasing global antibiotic consumption, poor surveillance and early warning system, and weak pipelines for new antibiotics, have left everyone dangerously vulnerable and unprepared to a pandemic of resistant and untreatable infections. The shortcomings of the current global governance structure on AMR and its funding challenges must be overcome to prevent and prepare for future pandemics. Whether a WHO convention, agreement, or other instrument is taken up to effectively address pandemic preparedness and response, such discussions should consider how such investments can pay double dividends by systematically addressing antibiotic resistance.
Further reading
ReAct-Europe briefing note The-Pandemic Treaty and antibiotic resistance
Antibiotic Resistance Coalition: Global Action Plan on AMR – Review briefing (PDF)
Lancet: Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis
IACG discussion paper: Future Global Governance for Antimicrobial Resistance (PDF)
ReAct article: The world needs new antibiotics – so why aren’t they developed?
More from "Globally coordinated governance needed"
- A call for global action
- Toolbox – A guide for health care professionals
- Rational use of antibiotics
- Infection Prevention and Control
- Promoting rational use of antibiotics – the Thailand example
- Caring about antibiotic resistance is similar with reducing the plastic waste or saving water
- Systemwide response to antibiotic resistance requires effective and sustainable global governance