2017-10-12
It is well-known that antibiotic resistant infections have a major influence on the health of people globally. Antibiotic resistance increases both mortality and morbidity due to treatment failures and lack of effective therapy.
But antibiotic resistance has even more far-reaching consequences on different levels that often tend to be overlooked. The economic consequences may even be devastating, as increased treatment costs drain funds, morbidity and mortality affect the possibility to make a living and both of these drive inequality.

Poverty dimension of antibiotic resistance and its containment.
Agreed in 2015 by the 193 Member States of the UN, the new global agenda with Sustainable Development Goals (SDGs) offers an ambitious 15-year trajectory for the world’s sustainable development. Importantly, if unchecked antibiotic resistance threatens to undermine the achievements gained during the preceding Millennium Development Goals and can make the realization of many SDGs impossible. Here, as we commemorate October 17 as the Eradication of Poverty day, the micro- and macroeconomic dimensions of inaction on and containment of antibiotic resistance, respectively, are more than relevant.

International Day for the Eradiction of Poverty 2018
This year’s theme: “Coming together with those furthest behind to build an inclusive world of universal respect for human rights and dignity”.
This year marks the 70th anniversary of the proclamation of the Universal Declaration of Human Rights.
Read more about the day on United Nation’s website.
International Day for the Eradication of Poverty 2017
The Call to Action of October 17 was launched thirty years ago. This years theme is “Answering the Call of October 17 to end poverty: A path toward peaceful and inclusive societies”.
Antibiotic resistance and poverty on individual level
From an international development perspective, antimicrobial resistance strikes hardest at the poor. One-third of the world’s population do not have a safe toilet; more than 660 million people do not have access to clean drinking water, and one in every eight people currently defecates in the open. This leads to higher transmission of infections which in turn, and often avoidably and unnecessary, results in greater antibiotic consumption. Furthermore, such circumstances fuel drug resistance that does not only make infections harder to treat – it makes them more expensive to treat. This in return means that due to antibiotic resistance, effective treatment of many bacterial infections is out of reach for many people in low- and middle-income countries. With an increasing price for 2nd, 3rd-line treatment for multi-drug resistance organisms, it is relevant to consider the economic burden ABR puts on countries’ efforts towards health systems strengthening and Universal Health Coverage.
Many still pay for healthcare services and medicines solely out of their pockets. Antibiotic resistance makes the length of hospital stay increase hence more specialized and costly care is needed and more expensive drugs are being prescribed. For patients with limited resources, the accumulated costs may become insurmountable. As an example estimates from India state that the cost for treating a resistant bacterial infection is more than a years’ income for a rural worker. In addition to these direct costs for treatment, mortality and morbidity can drive the patient and family deeper into poverty due to loss of income. While a short-term loss of income may be possible to overcome, longer-term disability is more difficult and loss of a family supporter may be devastating. As a result of these pressures, Antibiotic resistance negatively impacts the economic performance of an individual which ultimately endangers progress towards SDG1 on ending poverty. Addressing ABR is, therefore, a direct prerequisite in poverty mitigation efforts.

Lack of affordable antibiotics
Median overall cost to treat a resistant bacterial infection in India is approx. $700 –> this is equivalent to 442 days of work of a rural male casual worker.
Source: Chandy S, Naik GS, Balaji V et al. High cost burden and health consequences of antibiotic resistance: The price to pay J Infect Dev Ctries. 2014 Sep 12;8(9):1096-102. doi: 10.3855/jidc.4745.
Antibiotic resistance and poverty on national level
As most countries secure the healthcare funding partially via national budgets, a significant proportion of the increased healthcare expenditure is directly incurred to the national economy and the country’s GDP. Additional healthcare costs linked to inpatients with antibiotic resistance infection, often due to required additional nursing and medical care, are becoming unbearable for both LMICs and high-income countries health expenditure budgets.
Furthermore, the cost toll due to antibiotic resistance reaches far beyond the health sector. It not only negatively influences the workforce economic outcomes directly, via decreased productivity, labor supply, and unemployment but drains out monetary resources from household income and tax revenues while creating an additional need for social services.

In OECD countries it is estimated that additional costs posed by antibiotic resistance per inpatient is equivalent to $10k-40k.
Source: Cecchini et al. ANTIMICROBIAL RESISTANCE IN G7 COUNTRIES AND BEYOND: Economic Issues, Policies and Options for Action. OECD. 2015
Macroeconomics of the issue
Without effective action, the issue of resistance is predicted to cause 10 million deaths annually and cost up to US$100 trillion by 2050. According to the World Bank’s report, ‘of the additional 28.3 million people falling into extreme poverty in 2050 in the high-impact antimicrobial resistance scenario, the vast majority (26.2 million) would live in low-income countries.’ Cost of inaction had been calculated to be at 1.1% to 3.8% decrease of global GDP by 2050. To put things into perspective, the consequences of climate change are predicted to cause a drop of 1.0% to 3.3% global GDP by 2060. Furthermore, US$23 billion of an additional health care spending will be needed in EU and US each year to fill the gap in addressing the issue of resistance. Such enormous costs may undermine efforts for sustainable economic growth as emphasized in SDG 8, making antimicrobial resistance a critical global development issue.
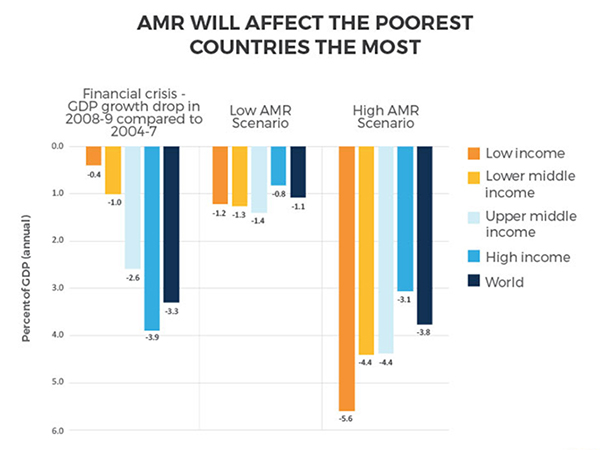
Antimicrobial resistance will affect the poorest countries the most
Compared to the fincancial crisis in 2008-2009 a high AMR scenario will affect almost all of us harder. And it will affect the poorest countries the most.
Source: World Bank. Drug-Resistant Infections: A Threat to Our Economic Future. 2017
The window of opportunity
Now, when the political and scientific linkages have been drawn between antibiotic resistance, poverty, and sustainable development, it is time to ‘walk the talk’. Containment of antibiotic resistance requires a multifaceted global response and lasting political will to pool and deploy technical and financial resources already today. Such undertakings represent a high-yield investment with the annual rate of return estimated to be reaching up to 88% per year.
References
Laxminarayan R, Duse A, Wattal C, et al. Antibiotic resistance-the need for global solutions. Lancet Infect Dis. 2013;13:1057–98.
Smith RD, Yago M, Millar M, Coast J. Assessing the macroeconomic impact of a healthcare problem: the application of computable general equilibrium analysis to antimicrobial resistance. J Health Econ. 2005;24:1055–75. (Paid content)
Review on Antimicrobial Resistance. Tackling a crisis for the health and wealth of nations. London, United Kingdom 2014.
Chandy S, Naik GS, Balaji V et al. High cost burden and health consequences of antibiotic resistance: The price to pay J Infect Dev Ctries. 2014 Sep 12;8(9):1096-102. doi: 10.3855/jidc.4745.
Cecchini et al. ANTIMICROBIAL RESISTANCE IN G7 COUNTRIES AND BEYOND: Economic Issues, Policies and Options for Action. OECD. 2015
World Bank. Drug-Resistant Infections: A Threat to Our Economic Future. 2017
