2019-02-19
Knowledge is critical for good policy and practical work. In the Global Action Plan on AMR adopted by WHO in 2015, strategic objective 2 is to “Strengthen the knowledge and evidence base through surveillance and research”. But how can this be done in countries that lack funds and technical capacity?
Good surveillance data gives information about for example how common resistance is in different settings and pathogens, trends of resistance development and can provide valuable input to the development of local and national policies and guidelines, strengthen investment cases for AMR, as well as increasing accountability and monitoring progress of AMR response. While the plan specifically discusses surveillance on antimicrobial resistance, surveillance is also needed for other related areas as well like antimicrobial use. Building capacity and systems will be essential for country level surveillance of resistance and consumption data. The ad hoc Interagency Coordination Group on Antimicrobial Resistance (IACG), in their draft recommendations, note that there is an urgent need to strengthen surveillance frameworks and capacity. Complementary data collection approaches will be important where there is not yet capacity to develop surveillance systems.
The global antimicrobial surveillance system
As a response to the need of surveillance, WHO has launched the global antimicrobial surveillance system, GLASS. The system has already started collecting data and published an early implementation report giving information about the status of the system in 40 countries as well as data from 22 countries. The major drawback of surveillance systems is however that they tend to be “heavy” – they require laboratory capacity to screen hundreds of bacteria with standardized methods on a regular basis. Samples need to be collected, transported, analyzed and reported to the national coordinating centre. If healthcare and laboratory structures are not already in place, this is a major undertaking. This is also reflected in the early implementation report, where most European countries have well developed surveillance systems that have been gradually built over many years of reporting to EARS-Net and its predecessor EARSS since 1998. However, many low income countries only have few surveillance sites reporting to the coordinating centre.
Point prevalence studies
A less resource intensive method for gathering similar data is through point prevalence studies. By definition, point prevalence studies gather data during a specified point in time, such as number of inpatients with infections caused by multidrug resistant bacteria. This gives a snapshot image of the situation in the studied location, which could be a hospital ward, whole country or even global. Depending on the study design, information captured can include for example bacterial species, resistance determinants, antibiotic use, guideline adherence or hospital acquired infections.
Global PPS on antimicrobial consumption and resistance
An example of point prevalence studies is the Global PPS project which is coordinated at the University of Antwerp. Within the scope of the project, point prevalence surveys have been performed since 2015. In the first report published in 2018, data was gathered from 303 hospitals in 53 countries, and the number of participating hospitals has increased since then. The project is based on voluntary reporting of data via a web-based form making participation simple. Once data has been uploaded, the participant can download their own data at any time in spreadsheet format. Ownership to the data is retained by the reporter.
Urgently needed data at low cost
Comparing with setting up a surveillance system, a point prevalence survey can provide a manageable way of collecting data on antibiotic resistance. The studies can be performed by a healthcare facility, an academic research group or even ministries of health at relatively low cost and without causing major infrastructural challenges. In the case of antibiotic resistance, samples could even be taken at the healthcare facility and then be transported to e.g. a research laboratory for analysis. Even though the collected data is not possible to submit to for example GLASS, a high quality point prevalence survey will give sufficient data to inform policy makers, guideline creators and individual prescribers. This is data that is needed directly and should not await the creation of surveillance systems.
Further reading
More news and opinion from 2019
- ReAct’s 2019 wrap up and 2020 expectations
- Blog post by UNDP and ReAct: Antimicrobial resistance: An emerging crisis
- Water, sanitation and hygiene services critical to curbing antibiotic quick fix
- Diagnostics: Antibiotic susceptibility
- ReAct highlights during World Antibiotic Awareness week 2019
- 2019 AMR photo competition prizes announced
- Launch of UNICEF’s institutional guidance on antimicrobial resistance
- Proposed ban on colistin for animal use announced in Indonesia
- School children led celebration of World Toilet Day and World Antibiotic Awareness Week
- 10 Innovate4AMR-winning teams enjoyed 3-day workshop in Geneva
- After 4 collaborative meeting days: Actions for the future in Latin America
- Four key points from joint comments to One Health Global Leaders Group on AMR
- Why are children more vulnerable to AMR?
- Dr Yoel Lubell, Health Economist, on Thailand, AMR, UCH and cultural factors driving AMR
- UHC and AMR: The Thai Experience
- Why do effective antibiotics matter for quality of care and patient safety?
- New ReAct policy brief: Antimicrobial resistance and universal health coverage – What’s the deal?
- Three key takeaways from the ReAct Africa conference
- Diagnostics: Species identification
- AMR-specific indicator proposed for monitoring Sustainable Development Goals
- Five focus areas at the 2nd Ministerial Conference on AMR hosted by the Netherlands
- Safety concerns of fecal microbiota transplants
- Upcoming ReAct Africa Conference: universal health coverage and antimicrobial resistance in focus
- Mother Earth conference in Argentina – the environment in focus
- Diagnostics: What are we talking about?
- Connecting global to local civil-society-agenda on AMR at CSO convening in Geneva
- ReAct colleagues featured in WHO Bulletin as leading profiles in the work on reacting to antibiotic resistance
- RAN stakeholder at WHO IPC consultation – for standards and guidelines in African Union member states
- WHA conversation on Antibiotic Resistance as a Global Development Problem co-organized by ReAct
- Insights from ReAct Asia Pacific project on antibiotic stewardship in secondary level hospitals in India
- Open letter to UN Member States from former IACG members Anthony So and Otto Cars
- ReAct UHC Intervention at UNGA Multi-stakeholder Hearing for High-level Meeting on UHC
- ReAct Latin America honors Earth Day
- Medicines Patent Pool’s view on the role of licenses for antibiotics – World Intellectual Property Day
- Second time for Innovate4AMR competition!
- World Health Day 2019: Universal Health Coverage
- Diagnostics: Constraints for successful implementation
- Antibiotic Shortages: magnitude, causes and possible solutions: A new WHO meeting report
- Erry Setyawan, FAO, on Indonesian NAP: We need to work together to make it possible to manage AMR
- ReAct’s new 5-year strategic plan receives funding from Sida
- How infections spread and how to stop them
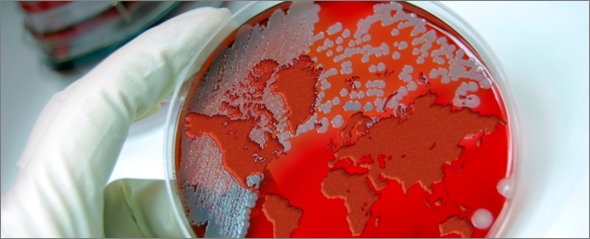
- Generating data for policy and practice
