2020-02-20
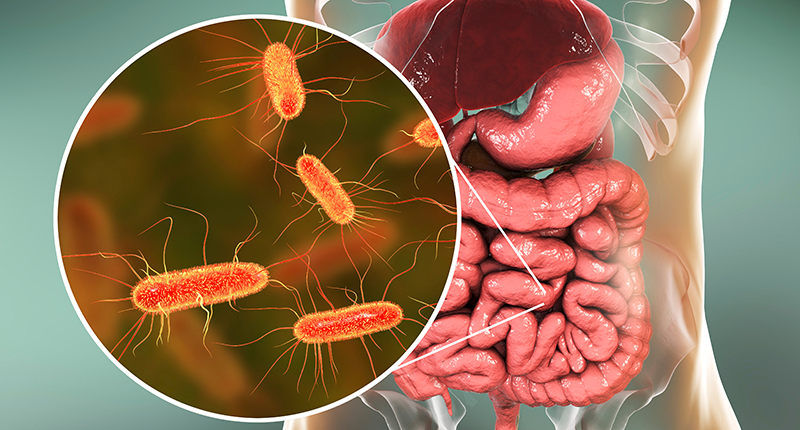
What is the relationship between the bacteria in us and our health? And can these bacteria cause diseases that we think are noncommunicable? In 2017, ReAct published a factsheet on the human microbiome that brought up some of these connections, but today we know even more as research has moved forward.
Difficulties of microbiome-related disease research
In the past, knowledge of our microbiomes has been greatly hampered by research methods that have restricted our knowledge to a fraction of the bacterial species that inhabit our bodies, namely the species that we are able to culture in a lab. With newer methods, many of these previously unknown species can now be detected, at least on a molecular level. Also, Koch’s postulates have been ingrained into generations of microbiologists as requirements to be filled in order to infer that a specific bacterium causes disease. While these postulates are known to have limitations, they can still be seen as a framework to understand microbial causes of disease.
Koch’s postulates
In 1890, the German microbiologist Robert Koch published four postulates to determine if a microorganism causes disease:
- The microorganism must be present in all cases of the disease.
- The microorganism can be isolated from the diseased host and grown in pure culture.
- The microorganism from the pure culture must cause the disease when inoculated into a healthy, susceptible laboratory animal.
- The microorganism must be re-isolated from the new host and shown to be the same as the originally inoculated microorganism
Our microbiomes are now understood to be complex ecosystems of a large variety of bacteria. Many diseases have been associated with changes (called dysbiosis) in these ecosystems rather than the lack or excess of a specific species. Generally dysbiosis leads to decreased diversity, with fewer different species flourishing in the microbiome. It is however important to remember that correlation does not imply causation.
Correlation or causation?
In studies of the connection between microbiomes and diseases, dysbiosis may correlate with a disease. This means that when dysbiosis is present, in general so is the disease. This does however not mean that the dysbiosis causes the disease. It is equally possible that the disease could cause the dysbiosis. It could even be that there is a third factor, such as our diet, that causes both the dysbiosis and the disease.
A way to be able to make the causal inference is therefore needed. An explanation of the mechanism can be crucial component of this inference, but is often notably lacking. But even if there is a mechanistic explanation, our diet and living habits affect our microbiomes and may still be the ultimate cause of disease.
Examples of microbiome-related diseases
Many diseases have been suggested to be related to our microbiomes. Here, we take a quick look at three of them.
Obesity
Obesity is perhaps the first and most well studied disease connected to our microbiomes. Transplanting microbiomes from obese humans to laboratory mice without microbiomes render the mice obese. Transplanting microbiomes from lean humans does not cause obesity. Studies of microbiomes show that microbiomes from obese people contain more bacteria of the phylum Firmicutes and less bacteria belonging to Bacteroidetes. Several mechanisms have been proposed to explain how the microbiome affects obesity: that the bacteria can increase energy uptake by increased fermentation of dietary fiber; that bacteria suppress a liver enzyme that regulates fat metabolism; or that the bacteria cause an inflammation reaction which in turn alters metabolism.
Cardiovascular disease
Cardiovascular disease is connected to a smaller difference in the microbiome – the bacterial genus Collinsella has been shown to be more common in patients with atherosclerosis that causes symptoms than in the control group. It’s uncertain if this genus of bacteria is connected to the proposed mechanism that increased levels of the bacterial product TMAO is connected to increased risk of cardiovascular disease.
Type 2 diabetes
Type 2 diabetes has also been studied for potential connections to the microbiome. Dysbiosis, as in lesser diversity and a shift in the relative abundance in Firmicutes and Bacteroidetes, like in the case of obesity, has been described. These microbiome changes cause inflammation that in turn contribute to the development of diabetes.
Kochs postulates redeemed?
A major obstacle for understanding microbiome-related noncommunicable diseases is the former strong emphasis on a single microorganism as the causative agent of disease. But what if we would view the whole ecosystem as being the cause of disease? This could indeed redeem the postulates to a certain extent, albeit not fully. Current knowledge of the microbiome and noncommunicable diseases indicates that where there is a connection, dysbiosis is a risk factor for development of disease. How much dysbiosis contributes, and how large the risks are compared to other risk factors, will continue to be debated in the foreseeable future.
Microbiomes and antibiotics
Every time we use antibiotics, whether to treat or prevent diseases, we also affect our microbiomes. While the most notable effects are seen with broad-spectrum antibiotics that sometimes cause a secondary infection with Clostridioides difficile, all antibiotics cause at least a temporary dysbiosis. Antibiotic use in pregnancy and early in life may have even more severe repercussions that we still do not fully understand. This raises an interesting question – if dysbiosis causes non-communicable diseases, and antibiotic use causes dysbiosis, how does this affect our use of antibiotics? Should antibiotic use be restricted not only due to the risk of resistance development, but also due to adverse events in the sense of increased risk for noncommunicable diseases?
Further reading
ReAct material: Microbiome factsheet
ReAct Toolbox: Bacteria – essential for human life
Clinical Nutrition Experimental: Gut microbiota and obesity
Science Magazine: Are noncommunicable diseases communicable?
More news and opinion from 2020
- Nurse Dorce, Indonesia: Treating small patients with much love and infection prevention – a success story
- ReAct highlights during World Antimicrobial Awareness week 2020
- ReAct Asia Pacific: Winners of 2020 photography competition
- WAAW ReAct Africa: Engaging civil society and students
- WAAW in Indonesia: Focus on One Health approach to AMR
- Innovate4Health’s 32 finalist teams: For social innovations to address emerging infectious diseases!
- ReAct Open Letter: 5 key points to One Health Global Leaders Group on Antimicrobial Resistance
- New ReAct Report: Treatment of newborn sepsis is threatened – effective antibiotics essential
- Upcoming ReAct Africa Conference: What is the status of the NAPs on AMR in the African region?
- Animal welfare and antibiotic resistance in food animals
- ReAct activities for World Antimicrobial Awareness Week 2020
- Dr. Honar Cherif: My patients can receive 5-10 courses of antibiotics during their cancer treatment
- New ReAct Report: Antibiotic resistance affects men and women differently
- ReAct Asia Pacific: Photo competition for students – health in focus
- 4 take aways from WHO’s first global report on sepsis
- Launch of global student design sprint – Innovate4Health
- World Sepsis Day – antibiotics essential in treatment of sepsis
- The new Pharmaceutical Strategy for Europe – an opportunity to put public interest first
- 4 key reflections on the recently launched WHO GLASS-report
- Key points from ReAct’s comments to the Independent Panel on Evidence
- ReAct Interview: From zoologist to community engagement on AMR
- ReAct Africa expands
- COVID-19 resolution – a missed opportunity to address global pandemic response more broadly
- What everyone needs to know about clinical research
- New ReAct Policy Brief: Successful cancer treatment relies on effective antibiotics
- Impact of COVID-19 on vaccine-preventable diseases and antibiotic resistance
- ReAct Africa and Africa CDC: COVID-19 webinars
- Antibiotic pollution: India scores a global first with effluent limits
- COVID-19 and AMR – what do we know so far?
- Learning from bedaquiline in South Africa – comprehensive health systems for new antibiotics
- ReAct Interview: How does antibiotics in food animal production end up in the environment?
- Key take aways from CSO workshop on AMR in Kenya
- New fact sheet: Effective antibiotics – essential for childrens’ survival
- Shortages and AMR – why should we care? 4 consequences of antibiotic shortages
- Our microbiome and noncommunicable diseases
- The 2020 AMR Benchmark Report – concerning findings with questionable framing
- 4 key reflections from engaging hospitals in India for antibiotic stewardship
- Teacher Gustavo Cedillo, Ecuador, teaches children about the bacterial world
