2018-04-07
On World Health Day, it is interesting to remind us all of the rise and approaching fall of one of the most powerful discoveries in medical history – antibiotics. What makes them so special, and why is bacterial resistance such a major threat to human health?
A brief history of medicine
Life expectancy in different regions in the world started to increase somewhere between the 1870´s and 1920’s. But why? One important factor is decrease in child mortality, but that’s not all. Life expectancy has also increased for those who survive childhood. The issue is of course complex, and any answers will reflect the viewpoint of the analyst. So let’s look at it from the perspective of infectious diseases. For example in the USA, the rate of mortality due to infectious diseases was 579.6 deaths/100,000 population or one third of all deaths in the year 1900, and the top three causes were all infections – some of them considered banal in the current western society. In 1998, only pneumonia and influenza made the top 10 list at #6 with a mortality rate of 34 deaths/100,000 population. Top three causes of death were heart diseases, cancers and cerebrovascular diseases (e.g. stroke) – together causing 527.1 deaths/100,000 population or roughly 60% of all deaths according to statistics from the CDC. Similar data from low income countries may be difficult to come by, but in e.g. India the main causes of death are cardiovascular diseases, respiratory diseases and tuberculosis – in that order – whereas Kenya reports HIV/AIDS, lower respiratory tract infections and diarrhea to be the top three killers.
A substantial part of the increase in life expectancy appears to be attributable to a decline in infectious disease mortality. In part this decline is caused by antibiotics, but that’s not the full story: life expectancy started increasing in the 1870’s, while the first antibiotics were discovered by Paul Erlich (arsphenamine in 1909) and by Sir Alexander Fleming (penicillin in 1928). Instead, one needs to look further back in the history of medicine and the works of e.g. Ignaz Semmelweiss (1818-1865), Louis Pasteur (1822-1895), Robert Koch (1843-1910) and Joseph Lister (1827-1912), who all made significant contributions to understanding the role of microbes and hygiene in medicine. In their time, surgery was not only extremely painful due to the lack of anesthesia, but also highly risky due to the risk of infections in wounds. Popular accounts also state that the main cause of death in wars was not combat but infections – both in wounds and due to unsanitary conditions in the fields.
Negative health effects of antibiotics?
While antibiotics may have been a success story like no other in the history of medicine, there are also downsides. The last decades have seen an increased interest in the ecosystem that we carry within us – the microbiome. As antibiotics do not discriminate between pathogens and beneficial bacteria, exposure to antibiotics has profound effects on the microbiome. The research field is difficult, and it is difficult to learn about the intricate interdependencies between us and our bacteria. But there are increasing amounts of evidence suggesting that antibiotic use could be at the heart of some of our modern epidemics such as asthma, allergies and obesity.
A world without antibiotics?
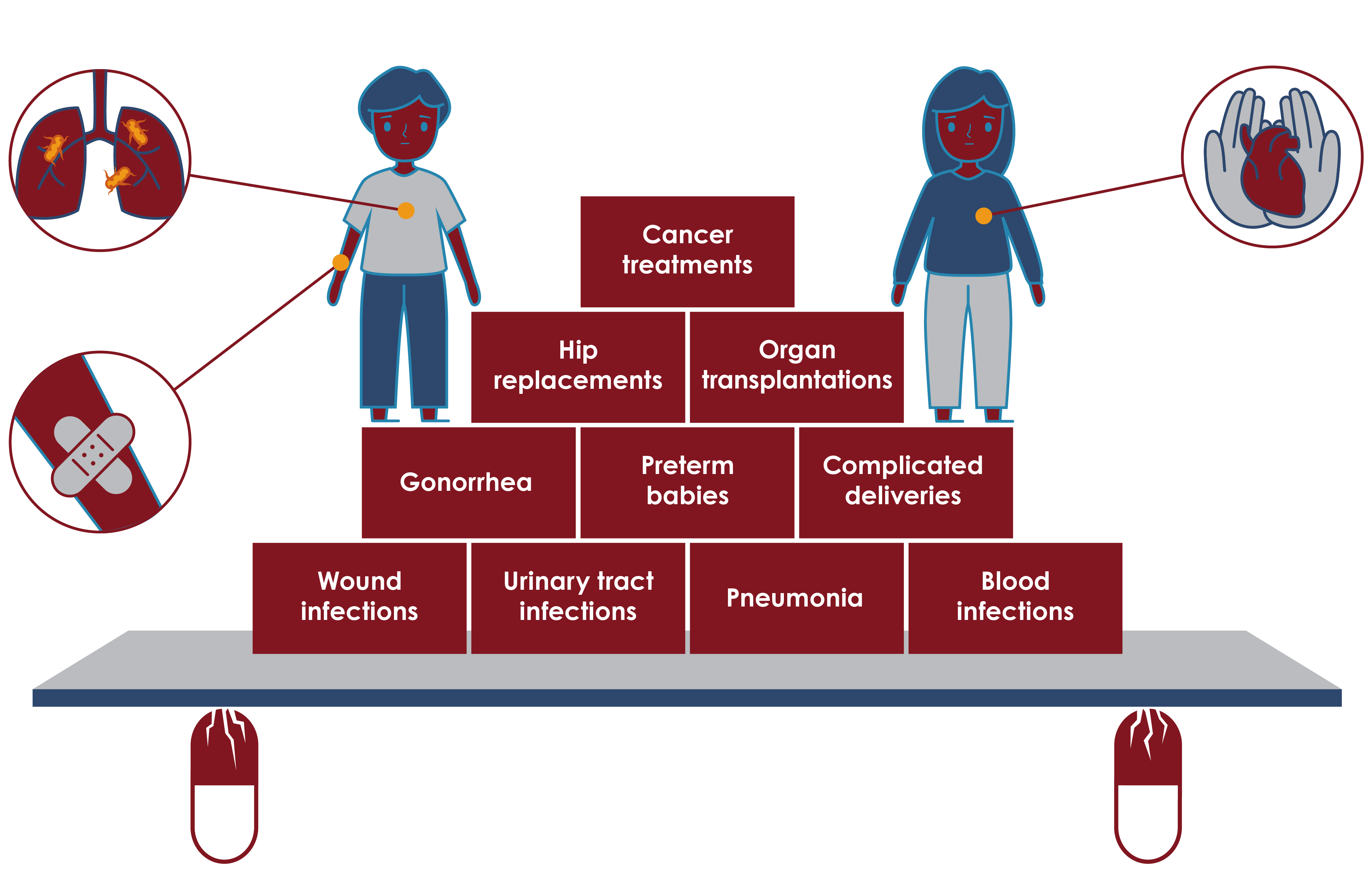
It is difficult to envisage a world without antibiotics – they are at the same time both a crucial component of healthcare and very much taken for granted. The UK Review on Antimicrobial Resistance that released its final report in 2016 estimates that if all antimicrobials (i.e. antibiotics, antifungals, antivirals and antiparasitals) are lost, this alone would cause 10 million deaths annually in 2050, and cause a USD 100 trillion cumulative loss in global GDP. While the actual numbers in the estimates can surely be criticized, it seems evident that the potential loss of antibiotic efficacy will have a dramatic effect on medicine:
- Many childhood and maternal infections could become fatal once again such as pneumonia and childbed fever – as they still are in many countries with limited access to antibiotics.
- Non-vital surgery would become difficult to justify due to the risk of infection.
- Most cancer therapies would become difficult to justify as chemotherapy causes immune suppression and increases the risk of even banal infections becoming fatal.
- Other therapies that require immune suppression, such as organ transplants will be untenable.
- “Ordinary” infections, such as wound infections, urinary tract infections and pneumonia will increasingly be associated with a risk of death.
For most parts of the world, there would be a decrease in life expectancy. Of course, this is already the normal state of affairs in many low income countries that struggle with weak health care systems and poor access to our current antibiotics. So life expectancy shouldn’t decrease to the levels of the preantibiotic era, as there have been major advances in water, sanitation and hygiene (WASH), infection prevention and vaccines. But the decrease would probably be significant – one might argue that a reasonable estimate would be to the early 21st century expectation in Africa, i.e. around 50-60 years.
An economic case for increased investment in antibiotic research?
It is obvious that both sustainable use of existing antibiotics and development of new efficient antibiotics are needed in order to maintain the advances of modern medicine. While many point to the poor return on investment for antibiotics as a reason for the decline in antibiotic development, there may be an economical argument to be developed from the above statistics.
Let’s assume the following:
- In a world without effective antibiotics, global life expectancy would drop to approximately 50 years.
- In a world without effective antibiotics, infectious diseases would again become the major causes of death globally.
- The major sources of revenue for the pharmaceutical industry are medicines against cancer, cardiovascular diseases and other chronic diseases that require long-term therapy and as such are mainly sold to the population aged 40 or older.
From these premises follow that in a world without effective antibiotics, pharmaceutical industry revenue (with their current portfolios) will be dramatically lower. While this argument acts on a longer time-scale than business usually does, it is thought provoking.
World health and antibiotics
It appears evident that progress in human health and wellbeing has historically gone hand in hand with decreasing the burden of infectious diseases, and that access to effective antibiotics are of paramount importance in this. While much has been achieved, much more can be done, and the shadow of the post-antibiotic era lurks gloomily in the near future. This is also at the heart of ReAct. The world needs global collective action to ensure equitable and sustainable access to antibiotics, discovery of new antibiotics to treat resistant infections and measures to reduce unnecessary use of antibiotics and thereby to preserve antibiotic efficacy. Only then can we achieve a world free from fear of untreatable infections.
Resources
Our world in data: Life Expectancy
CDC: Leading Causes of Death, 1900-1998